We need you! Join our contributor community and become a WikEM editor through our open and transparent promotion process.
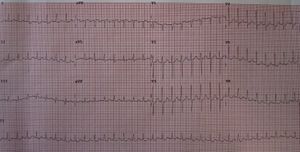
Paroxysmal supraventricular tachycardia
From WikEM
SVT terminology can be confusing, as some references consider SVT to be any rhythm originating above the ventricles (e.g. sinus tachycardia, MAT, atrial flutter, atrial fibrillation, PSVT, etc). As these entities have their own specific articles and treatment, only paroxysmal supraventricular tachycardia links here.
Contents
Background
- Also known as PSVT and frequently referred to just as SVT
- AV nodal reentrant tachycardia (AVNRT) and AV reentrant tachycardia (AVRT) are subtypes of PSVT
- Most common dysrhythmia in children
Clinical Features
- Palpitations
- Chest pain, fatigue, diaphoresis
- May also present with hemodynamic instability if severe (e.g. hypotension, syncope)
- Infants: poor feeding, tachypnea, irritability
Differential Diagnosis
Palpitations
- Arrhythmias:
- Atrial fibrillation
- Grouped beats on ECG (commonly misdx as A-fib)
- Atrial bigeminy and trigeminy
- Mobitz I or Mobitz II
- Atrial flutter
- SVT
- Ventricular Tachycardia
- Sick sinus syndrome
- Multifocal atrial tachycardia
- PVCs
- Wolff–Parkinson–White syndrome (WPW)
- Sinus node dysfunction
- AV Block
- Lown-Ganong-Levine Syndrome
- Accelerated idioventricular rhythm
- Non-arrhythmic cardiac causes:
- Cardiomyopathy
- CHF
- Mitral valve prolapse
- Congenital heart disease
- Pericarditis
- Valvular disease
- Pacemaker malfunction
- Acute MI
- Psychiatric causes:
- Drugs and Medications:
- Alcohol
- Caffeine
- Meds (i.e. digitalis, theophylline)
- Street drugs (i.e. cocaine)
- Tobacco
- Misc
Evaluation
| Symptoms | Sinus tachycardia | SVT |
| History | Volume loss | Sudden onset |
| Physical Exam | Dehydrated | CHF-like |
| ^Heart Rate (generally) | <180 | >180 |
| Variability | Yes | No |
^In infants HR cuttoff = 220
- ECG findings
- P-waves
- Sinus tachycardia - may be seen before QRS complexes
- SVT - either p-waves not seen OR retrograde p-waves
- Signs with no actionable clinical relevance, unless they persist after conversion
- ST depressions in any lead
- ST elevation in aVR
- P-waves
- Consider PSVT underlying causes to include[1]:
- Drug toxicity, especially caffeine, stimulants, digoxin
- EtOH
- Thyroid disease
- Electrolyte abnormality
- Hypoxia, pulmonary embolism
- Pre-existing heart disease (prior MI, MVP, pericarditis)
- However, SVT is very rarely isolated manifestation of ACS
- Evaluate signs and symptoms as if there is no dysrhythmia
- Ensure resolution of ST changes found during PSVT episode
- Generally, troponins are not indicated in patients without significant risk factors for CAD[2]
Unstable Management
- Synchronized cardioversion 0.5-1.0 J/kg
- Pediatrics: cardioversion at 0.5-1 J/kg. If unsuccessful, increase to 2 J/kg
- Consider giving sedation prior to cardioversion if it will not significantly delay the procedure
Stable Management
Vagal maneuvers
- Modified Positional Valsalva more successful than normal Valsalva maneuver[3]
- Consider having legs all the way over the patient's head, which is even more than the [[modified positional valsalva, if patient can tolerate[4]
- Pediatrics: often successful with ice application to face
- Carotid sinus massage (ideal duration of 15 seconds[5])
- Auscultate to rule out bruits in carotid artery before performing
- Perform ONE side at a time
Adenosine
- Adults: 6mg IVP (1st dose) → 12mg (2nd dose) IV push (if initial dose fails)
- Pediatrics: 0.1mg/kg (1st dose) → 0.2mg/kg (2nd dose) IV push (if initial dose fails)
- Contraindicated in asthmatics
- Some literature to support 3rd dose of 18mg if 12mg fails[6]
- May decrease initial dose to 3mg if[7]:
- Central line
- Heart transplant
- Taking carbamazepine or dipyridamole
Calcium-channel blockers
Adults
- Diltiazem 15–20mg IV over 2min
- May give 25mg IV if inadequate response after 15min
- If IV bolus worked start IV infusion at 5–20mg/hr
- Contraindications: Hypotension, CHF, any suspicion of VT
- Consider calcium gluconate premedication OR afterwards if BP falls
Pediatrics
Beta-blockers
Adults
- Metoprolol 5mg IV q5min x 3; give 50mg PO if IVP effective
- Esmolol 500mcg/kg IV over 60sec
- May give repeat bolus if inadequate response after 2-5min
- If effective start infusion at 50mcg/kg/min (titrate up to 300mcg/kg/min)
Pediatrics
- Propranolol 0.3-1mg/kg q6hrs IV (contraindicated in asthmatics)[8]
- Atenolol 0.5-1mg/kg q12hrs (caution in asthmatics)[8]
Disposition
- Most can be discharged
- Avoid stimulants, sympathomimetics
- Consider low dose beta-blocker prescription, beta-1 specific (atenolol, metoprolol)
- Follow up with primary care provider if first episode
- Follow up with cardiology if recurrent episodes
- A retrospective review of 111 patients found[9]:
- 79 (71%) were discharged from the ED
- 3 (4%) in this group had recurrent SVT after discharge
- None had an unstable event
- 32 (29%) were admitted to the hospital
- 6 of the 32 (19%) had recurrent PSVT in the hospital
- Recurrence more likely to occur in older patients and those with CVD
- 79 (71%) were discharged from the ED
See Also
External Links
Amal Mattu ECG Case: Feb 26 2012
References
- ↑ Gugneja M et al. eMedicine. Paroxysmal Supraventricular Tachycardia. Dec 30, 2015. http://emedicine.medscape.com/article/156670-overview#a5.
- ↑ Bukkapatnam et al. Relationship of myocardial ischemia and injury to coronary artery disease in patients with supraventricular tachycardia. Am J Cardiol. 2010 Aug 1;106(3):374-7.
- ↑ Appelboam A. et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial fulltext
- ↑ Schwartz AC. News: An Effective Maneuver to Break PSVT. Emergency Medicine News: March 2017 - Volume 39 - Issue 3 - p 28.
- ↑ Appelboam, A, et al. Randomised Evaluation of modified Valsalva Effectiveness in Re-entrant Tachycardias (REVERT) study. BMJ, 2014; 4(3):e004525.
- ↑ Weismuller P et al. Terminating supraventricular tachycardia with adenosine--comparing the effectiveness of 12mg and 18mg. Dtsch Med Wochenschr. 2000 Aug 18;125(33):961-9.
- ↑ ACLS Algorithms. https://acls-algorithms.com/acls-drugs/acls-and-adenosine/.
- ↑ 8.0 8.1 8.2 Salerno, J et al. Supraventricular Tachycardia Arch Pediatr Adolesc Med. 2009;163(3):268-274.
- ↑ Luber S, Brady WJ, Joyce T, et al. Paroxysmal supraventricular tachycardia: outcome after ED care. Am J Emerg Med. 2001; 19(1):40-42.