Reporting, Data Collection, and Findings
Reporting to the US Zika Pregnancy Registry
- Healthcare providers should report women and infants who are eligible for the US Zika Pregnancy Registry to their state, local, tribal, or territorial health departments. If CDC USZPR staff receive reports directly from healthcare providers, health departments will be notified.
- Health department staff can submit information to CDC USZPR staff by
- CDC Secure Access Management Services (SAMS) (contact CDC for access at ZikaMCH@cdc.gov)
- Electronic data transfer through FTP (e.g. CSV, Excel, Access, Word, PDF files) (contact CDC for access)
- Encrypted email to ZikaMCH@cdc.gov
- Secure fax at 404-718-1013
Data Collection
- Various methods (e.g., medical record abstraction, telephone consultation) can be used to collect surveillance information for the US Zika Pregnancy Registry. CDC has distributed data collection forms and other technical materials directly to health departments and provides ongoing technical assistance to assist with data collection. Healthcare providers should contact their state, tribal, local, or territorial health department to obtain data collection forms.
- Depending on preference and capacity of the state, tribal, local, or territorial health department, health departments may choose to collect USZPR information directly from healthcare providers or ask CDC staff for assistance.
- The USZPR uses several forms to collect information. Data elements on these forms are designed to capture information about routine clinical care for pregnant women and their infants and are not intended as recommendations for additional testing or management.
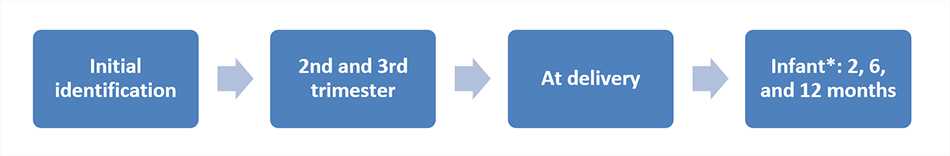
- If available, data should be collected at regular time points (see graphic below).
The USZPR collects follow-up information on all reported infants born to women with laboratory evidence of possible Zika virus infection (regardless of whether they have symptoms) and periconceptionally, prenatally, or perinatally exposed infants born to these women, including infants who appear healthy at birth. The inclusion of infants who appear healthy is important because the short-term and long-term effects of in utero exposure to Zika virus are unknown. The USZPR is collecting this information because the full range of potential fetal or infant effects of maternal Zika virus infection are unknown.
Communicating Findings from the US Zika Pregnancy Registry
- The cumulative number of pregnant women included in the US Zika Pregnancy Registry is reported on the CDC Zika website about twice a month. These reports reflect totals for the:
- 50 US states and District of Columbia (based on data from the Registry)
- US territories (based on data from the Registry and data from Puerto Rico reported to Zika Active Pregnancy Surveillance System (ZAPSS).
- CDC also reports poor outcomes of pregnancy among women with laboratory evidence of possible Zika virus infection from the Registry twice a month. These outcomes include
- Liveborn infants with birth defects and
- Pregnancy losses with birth defects
These reports will include birth defects consistent with current knowledge of the effects of congenital Zika virus infection, including microcephaly (a condition where a baby’s head is much smaller than expected) and other severe brain defects.
- Some data limitations should be considered when reviewing findings from the USZPR. Only pregnant women or infants who are tested for Zika virus infection and reported to the Registry are included. The USZPR will therefore reflect reported Zika virus infection and outcomes and could underestimate infection and outcomes to the extent that these are not reported. The USZPR is not designed to determine whether poor pregnancy outcomes in women who had possible Zika virus infection during pregnancy were caused by Zika virus or other factors.
Roles of Health Department and Healthcare Providers
Health departments and healthcare providers play a critical role in ensuring the success of the US Zika Pregnancy Registry. Specific roles for health departments and healthcare providers are summarized in the table below.
| Group | Identify pregnant women and infants who may be eligible for the USZPR | Report to the USZPR | Collect information about pregnancy and infant outcomes |
|---|---|---|---|
| Health Departments | Yes | Yes, report to CDC | Yes, collaborate with CDC |
| Healthcare Providers* | Yes | Yes, report to state, tribal, territorial or local health department | Yes, collaborate with state, tribal, territorial or local health department |
* Puerto Rico has established a separate Zika Active Pregnancy Surveillance System (ZAPSS). Healthcare providers practicing in Puerto Rico should report information to ZAPSS rather than the USZPR.
Coordination with Other Arboviral Disease Surveillance
- Zika virus disease and Zika virus congenital infection are nationally notifiable conditions and can be reported to ArboNET, CDC’s national arboviral disease surveillance system. The Council of State and Territorial Epidemiologists (CSTE) has interim case definitions [PDF – 11 pages] for Zika virus disease and congenital Zika virus infection. When finalized, the updated Zika virus CSTE position statement will be available here.
- ArboNET and the Registry are surveillance systems that address different public health needs and use different inclusion criteria.
- National estimates for pregnant women and infants identified with possible Zika virus infection from the Registry are different from the total numbers of people with reported Zika virus disease from ArboNET, which are also reported weekly .
- When Zika virus disease in a pregnant woman or congenital Zika infection in an infant is reported to ArboNET, CDC USZPR staff are notified, and they will capture data elements already reported through ArboNET to prevent duplicate reporting.
Protection of Health Information
- CDC takes the protection of confidential and sensitive information very seriously. CDC follows strict standards to ensure that the privacy of people whose health information we collect is protected. In addition, data in the US Zika Pregnancy Registry (the Registry) are collected in a way that ensures they are safeguarded against unauthorized disclosure. Information from the Registry will only be reported to the public in aggregate form. CDC will not release any identifiable data.
- CDC is requesting the collection of clinical information in identifiable form as a public health authority. As defined in the Health Insurance Portability and Accountability Act (HIPAA) and its implementing regulations, Standards for Privacy of Individually Identifiable Health Information (45 CFR § 164.501)] (“Privacy Rule”), covered entities (e.g., healthcare providers) may disclose protected health information without patient authorization to a public health authority that is authorized by law to collect or receive such information for the purpose of preventing or controlling disease (42 CFR 164.512).
- Data collected for the Registry include clinical information pertaining to the pregnant woman’s health, monitoring, and testing during pregnancy, results from evaluation and testing conducted at birth, and health information from the infant through the first year of life. As established in the HIPAA Privacy Rule (45 CFR 164.528), individuals have the right to request from covered entities (i.e., the healthcare provider) an accounting of the disclosures of their protected health information.
- The data in the Registry are protected by an Assurance of Confidentiality. An Assurance of Confidentiality is a formal confidentiality protection authorized under Section 308(d) of the Public Health Service Act. It is used for projects conducted by CDC staff or contractors that involve the collection or maintenance of sensitive identifiable or potentially identifiable information.
CDC has determined that the Registry is a non-research public health surveillance activity in the context of a public health emergency.
- Page last reviewed: October 3, 2017
- Page last updated: October 3, 2017
- Content source:




 ShareCompartir
ShareCompartir