AR Solutions in Action
Antibiotic Resistance (AR) Lab Network Established as New Fungal Threat Emerges

CDC is committed to supporting vital laboratory capacity in every state to rapidly detect new forms of antibiotic resistance through its Antibiotic Resistance Laboratory Network (AR Lab Network). The new network was established in 2016 with support from Congress. As new or rare forms of antibiotic resistance emerge, CDC’s AR Lab Network supports nationwide capacity to rapidly detect these threats in health care, food, and the community, and inform local responses to prevent spread and protect people. Read about one example of the AR Lab Network’s importance and early success, highlighted in its response to the emerging resistant fungus, Candida auris (C. auris).
C. auris: CDC’s Response to a Global Emerging Threat

Candida auris (C. auris) is an emerging multidrug-resistant yeast that can cause invasive infection and death. After learning from international partners that C. auris had spread between patients in their hospitals—which is unusual for Candida—CDC’s response was swift. Rather than waiting for C. auris to be reported in the United States, CDC released a Clinical Alert in June 2016 asking labs and healthcare workers to be on the lookout for C. auris, particularly because C. auris is often misidentified as a less-threatening germ. Knowing that a patient’s infection is caused by C. auris is key to prescribing the right treatment and stopping its spread. CDC continues to provide new information and guidance to healthcare workers and laboratories about C. auris. As part of this effort, CDC is intensively working with partners to investigate new cases and learn how to successfully contain and prevent C. auris infections.
Improving Antibiotic Prescribing with Rapid Diagnostics and Education

CDC estimates about 80 percent of patients with Valley fever are given one or more rounds of antibiotics to kill bacteria before receiving a correct diagnosis and appropriate treatment. But Valley fever is caused by a fungus so these types of antibiotics will not work! Taking antibiotics that are not effective can put people at risk for negative drug reactions and can allow more resistant and harmful bacteria to grow. CDC is working to improve awareness about Valley fever and supporting the development of rapid diagnostic tests. A rapid diagnostic test can provide clinicians with information to quickly diagnose patients, get them the correct treatment, and prevent the use of unneeded antibiotics.
CDC and Partners Tackle Drug-Resistant TB in India

Worldwide, there are at least 580,000 cases of drug-resistant tuberculosis (TB). We must address TB both at home and abroad to ensure a safer, healthier America. To protect Americans from threats like drug-resistant TB, CDC is reinforcing international collaborations and capacities for antibiotic resistance prevention, surveillance, and infection control with countries worldwide. This work includes improving TB infection control (prompt detection and separation of infected patients, airborne precautions, and personal protective equipment for healthcare personnel) in key healthcare facilities. CDC is also strengthening diagnostic and treatment services for TB in the public and private sector, and increasing TB treatment adherence to reduce rates and spread.
Newly Reported Gene, mcr-1, Threatens Last-Resort Antibiotics
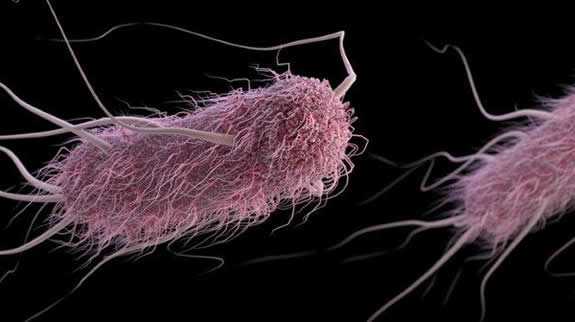 A new gene known as mcr-1— which can make bacteria resistant to colistin, a last-resort drug for some multidrug-resistant infections—was first reported in China in November 2015 and in the United States in May 2016. After the gene was discovered in bacteria from a patient in the United States, CDC and state and local health departments immediately launched a coordinated public health investigation to potentially prevent mcr-1 from becoming widespread in the U.S. Additional discoveries have been made, including those of two pigs in the United States, and further mcr-1 findings are expected.
A new gene known as mcr-1— which can make bacteria resistant to colistin, a last-resort drug for some multidrug-resistant infections—was first reported in China in November 2015 and in the United States in May 2016. After the gene was discovered in bacteria from a patient in the United States, CDC and state and local health departments immediately launched a coordinated public health investigation to potentially prevent mcr-1 from becoming widespread in the U.S. Additional discoveries have been made, including those of two pigs in the United States, and further mcr-1 findings are expected.
- Page last reviewed: July 6, 2016
- Page last updated: August 1, 2017
- Content source:


 ShareCompartir
ShareCompartir