Multistate Outbreak of Human Salmonella Chester Infections (Final Update)
NOTICE: This outbreak is over. The information on this page has been archived for historical purposes only and will not be updated.
Posted September 9, 2010
Outbreak Summary
CDC collaborated with public health officials in many states, the U.S. Department of Agriculture’s Food Safety and Inspection Service (USDA/FSIS), and the U.S. Food and Drug Administration (FDA) to investigate a multistate outbreak of Salmonella serotype Chester infections. Investigators used DNA analysis of Salmonella bacteria obtained through diagnostic testing to identify cases of illness that were part of this outbreak.
As of 9:00 AM EDT on August 27, 2010, a total of 44 individuals infected with a matching strain of Salmonella Chester have been reported from 18 states since April 11, 2010. The number of ill people identified in each state with this strain is as follows: AK (1), CA (5), CO (2), GA (8), IL (1), KY (1), MA (2), MN (2), MO (1), NC (1), OK (1), OR (2), SC (2), TN (1), TX (3), UT (3), VA (4), and WA (4). Among those for whom information is available about when symptoms started, illnesses began between April 4, 2010 and June 16, 2010. Case-patients ranged in age from <1 to 88 years old, and the median age was 36 years. Fifty-four percent of patients were female. Among the 43 patients with available hospitalization information, 16 (37%) were hospitalized. No deaths were reported.
The outbreak can be visually described with a chart showing the number of people who became ill each day. This chart is called an epidemic curve or epi curve. For more details, please see the Timeline for Reporting Cases of Salmonella Infection.
Outbreak Investigation
A widely distributed contaminated food product might cause illnesses across the United States. The identity of the contaminated product often is not readily apparent. In outbreaks like this one, identification of the contaminated product requires conducting detailed standardized interviews with persons who were ill. It may also require conducting interviews with non-ill members of the public (“controls”) to get information about foods recently eaten and other exposures to compare with information from the ill persons. The investigation is often supplemented by laboratory testing of suspected products.
Collaborative investigative efforts of officials in many local, state, and federal public health, agriculture, and regulatory agencies linked this outbreak to Marie Callender’s Cheesy Chicken & Rice single-serve frozen entrées. During June 14-18, 2010, CDC and public health officials in multiple states conducted an epidemiologic study by comparing foods eaten by 19 ill and 22 well persons. Analysis of this study suggested that eating a Marie Callender’s frozen meal was a source of illness. Ill persons (89%) were significantly more likely than well persons (14%) to report eating a frozen meal. All ill persons (100%) who ate frozen meals reported eating a Marie Callender’s frozen meal. None of the well persons who ate a frozen meal reported eating a Marie Callender’s frozen meal. There was insufficient data from this study to implicate a specific frozen meal type. However, many of the ill persons reported eating a Marie Callender’s Cheesy Chicken & Rice frozen entrée in the week before becoming ill. Additionally, two unopened packages of Marie Callender’s Cheesy Chicken & Rice single-serve frozen entrées collected from two patients’ homes (one collected in Minnesota on June 18, and one in Tennessee on July 19) yielded Salmonella Chester isolates with a genetic fingerprint indistinguishable from the outbreak pattern.
Recall Information
On June 17, 2010, ConAgra Foods announced a precautionary recall of Marie Callender’s Cheesy Chicken & Rice single-serve frozen entrées after being informed by the CDC of a possible association between this product and the outbreak of Salmonella Chester infections.
Clinical Features/Signs and Symptoms
Most people infected with Salmonella develop diarrhea, fever, and abdominal cramps 12–72 hours after infection. Infection is usually diagnosed by culture of a stool sample. The illness usually lasts 4 to 7 days. Although most people recover without treatment, severe infections can occur. Infants, elderly people, and those with weakened immune systems are more likely than others to develop severe illness. When severe infection occurs, Salmonella may spread from the intestines to the bloodstream and then to other body sites and can cause death unless the person is treated promptly with antibiotics.
More general information about Salmonella can be found here under Salmonella FAQs.
Advice to Consumers
- Salmonella is sometimes present in raw foods (e.g., chicken, produce, and spices) which can be used as ingredients in not-ready-to-eat frozen dinners.
- Consumers should follow the instructions on the package label of the frozen dinner. Conventional ovens are better at cooking foods thoroughly. Microwave ovens vary in strength and tend to cook foods unevenly.
- If you choose to cook the frozen dinner using a microwave, be sure to:
- Cook the food for the time specified for your microwave’s wattage.
- Let the food “stand” for the stated time, so cooking can continue.
- Use a food thermometer to make sure that it is fully cooked to an internal temperature of 165 degrees Fahrenheit.
- Individuals who think they might have become ill from eating a Marie Callender’s frozen dinner should consult their health care providers.
- Consumers who have Marie Callender’s Cheesy Chicken & Rice single-serve frozen entrées in their freezer should discard them or return them to their retailer for a refund.
- Consumers are urged to read and follow the preparation instructions on the label of all frozen entrees. If the package says “Do Not Microwave,” consumers should follow that instruction and use a conventional oven. Consumers should use a food thermometer to make sure the entrees reach at least 165 degrees Fahrenheit.
General Information
Additional Resources
CDC’s Role in Food Safety
As an agency within the U.S. Department of Health and Human Services (HHS), CDC leads federal efforts to gather data on foodborne illnesses, investigate foodborne illnesses and outbreaks, and monitor the effectiveness of prevention and control efforts. CDC is not a food safety regulatory agency but works closely with the food safety regulatory agencies, in particular with HHS’s U.S. Food and Drug Administration (FDA) and the Food Safety and Inspection Service within the United States Department of Agriculture (USDA). CDC also plays a key role in building state and local health department epidemiology, laboratory, and environmental health capacity to support foodborne disease surveillance and outbreak response. Notably, CDC data can be used to help document the effectiveness of regulatory interventions..
Final Case Count Map
Persons infected with the outbreak strain of Salmonella Chester, by state, as of August 27, 2010 (n=44)
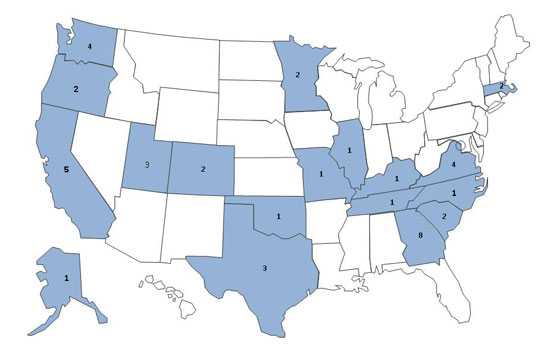
As of on August 27, 2010, a total of 44 individuals infected with a matching strain of Salmonella Chester have been reported from 18 states since April 11, 2010. The number of ill people identified in each state with this strain is as follows: AK (1), CA (5), CO (2), GA (8), IL (1), KY (1), MA (2), MN (2), MO (1), NC (1), OK (1), OR (2), SC (2), TN (1), TX (3), UT (3), VA (4), and WA (4).
Final Epi Curve
This outbreak can be visually described with a chart showing the number of persons who became ill each day. This chart is called an epi curve. Please see the Timeline for Reporting Cases of Salmonella Infection for more details on the reporting process.
Persons infected with the outbreak strain of Salmonella Chester, by week of illness onset*
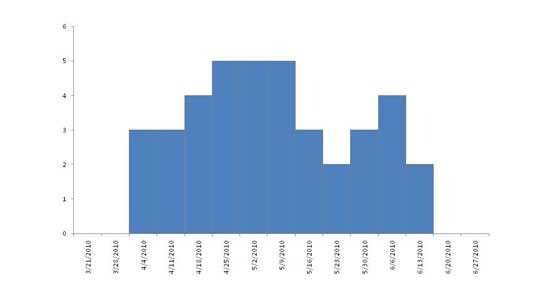
*n=44 for whom information was reported as of 08/27/10. Some illness onset dates have been estimated from other reported information.
- Page last reviewed: September 9, 2010
- Page last updated: September 9, 2010
- Content Source:


 ShareCompartir
ShareCompartir