Human Salmonella Typhimurium Infections Associated with Exposure to Clinical and Teaching Microbiology Laboratories (Final Update)
NOTICE: This outbreak is over. The information on this page has been archived for historical purposes only and will not be updated.
Posted January 17, 2012
Outbreak Summary
On October 30, 2010, PulseNet, the national molecular subtyping network for foodborne disease surveillance, detected a multistate cluster of Salmonella Typhimurium infections with a particular pulsed-field gel electrophoresis (PFGE) pattern and other genetic characteristics, referred to here as strain X. In December, the New Mexico Department of Health identified 3 ill persons infected with strain X. One was a student and the 2 others were children of students in microbiology courses held at two different community college campuses. CDC collaborated with public health officials in several states to investigate this multistate cluster of Salmonella Typhimurium infections associated with exposure to clinical and teaching microbiology laboratories. Investigators used DNA analysis of Salmonella bacteria obtained through diagnostic testing to identify cases of illness that might be related.
Between August 20, 2010 and June 29, 2011, a total of 109 individuals infected with strain X of Salmonella Typhimurium were reported from 38 states: AK (2), AL (4), AZ (4), CA (3), CO (1), FL (1), GA (6), IA (1), ID (2), IL (4), IN (2), KS (4), KY (4), MA (4), MD (3), MI (3), MN (9), MO (2), NC (1), ND (1), NE (2), NH (1), NJ (3), NM (3), NV (1), NY (4), OH (3), OK (1), OR (1), PA (9), SC (2), SD (1), TN (2), TX (1), UT (4), WA (5), WI (4), and WY (1). Among persons with available information, illness onset dates range from August 20, 2010 to June 14, 2011, 2011. Infected individuals ranged in age from less than 1 year to 91 years old, and the median age was 21 years. Sixty-one percent of patients were female. Twelve percent of patients were hospitalized. One death was reported.
The timeline of infections can be visually described with a chart showing the number of persons who became ill each day. This chart is called an epidemic curve or epi curve. Please see the Timeline for Reporting Cases of Salmonella Infection for more details. The expected baseline for strain X in PulseNet is approximately 0 to 4 cases reported per week. Beyond these cases, Salmonella is an important cause of human illness in the United States.
Investigation of the Outbreak
In an epidemiologic study conducted during February and March 2011, 32 ill persons answered questions about exposures during the days before becoming ill. Investigators compared their responses with those of 64 persons of similar age previously reported to state health departments with other illnesses (controls). Preliminary analysis of this study suggested that exposure to clinical and teaching microbiology laboratories was a possible source of illness. Illnesses were identified among students in microbiology teaching laboratories and employees in clinical microbiology laboratories. Ill persons (60%) were significantly more likely than control persons (2%) to report exposure to a microbiology laboratory in the week before illness began. Additionally, multiple ill persons reported working specifically with Salmonella bacteria in microbiology laboratories. The New Mexico Department of Health found that the strain isolated from patients was indistinguishable by PFGE pattern from a commercially available Salmonella Typhimurium strain used in laboratory settings. This commercially available strain was known to be present in several teaching or clinical laboratories associated with ill students or employees infected with the outbreak strain. These data suggest this strain was the source of some of these illnesses. Additionally, several children who live in households with a person who worked or studied in a microbiology laboratory became ill with the outbreak strain.
The investigation then focused on potential risk factors in microbiology laboratories that work with infectious agents like strain X of Salmonella Typhimurium. CDC collaborated with state and local health departments, the American Society for Microbiology , and the Association of Public Health Laboratories to conduct a survey to identify areas where improvements in biosafety and laboratory safety training can be made to prevent future illnesses. The survey was conducted with two groups in May 2011: staff from laboratories that had been associated with illness, and staff from laboratories that were not associated with illness.
Laboratory practices and settings appear to be largely similar across both groups, but several differences were found. Staff working at laboratories that were associated with illness were less likely to have knowledge of biosafety training materials. In comparison, staff working in laboratories that were not associated with illness were more likely to train students and staff on the signs and symptoms of infection with Salmonella when conducting safety training. Similar safety policies were in place across the different laboratories. However, some policies appeared to be more difficult to monitor and enforce, such as not allowing the use of handheld devices (e.g., cell phones or music players) at the laboratory work space.
Findings of this survey indicate that teaching and clinical microbiology laboratory instructors should enhance training of students and staff on biosafety measures necessary in the laboratory. For more specific information, see the Biosafety in Microbiological and Biomedical Laboratories manual, the Guidelines for Biosafety Laboratory Competency MMWR Supplement, or the Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories MMWR Supplement.
Clinical Features/Signs and Symptoms
Most persons infected with Salmonella develop diarrhea, fever, and abdominal cramps 12 to 72 hours after infection. The illness usually lasts 4 to 7 days, and most persons recover without treatment. However, in some persons, the diarrhea may be so severe that the patient needs to be hospitalized. Salmonella infection may spread from the intestines to the blood stream, and then to other body sites and can cause death unless the person is treated promptly with antibiotics. The elderly, infants, and those with impaired immune systems are more likely to have a severe illness from Salmonella infection.
Advice to Students and Employees in Clinical and Teaching Microbiology Laboratories
- Be aware that bacteria used in microbiology laboratories can make you or others who live in your household sick, especially young children, even if they have never visited the laboratory.
- If you work in a laboratory, it is possible for you to bring bacteria home through contaminated lab coats, pens, notebooks, and other items that you use in the microbiology laboratory.
- Avoid taking laboratory supplies outside of the laboratory to limit contamination.
- Persons working with any infectious agents, including Salmonella bacteria, must be aware of potential hazards, and must be trained and proficient in biosafety practices and techniques required for handling such agents safely, in particular, to:
- Wash hands frequently while working in and immediately before leaving the microbiology laboratory and follow proper hand washing practices. This is especially important to do before preparing food or baby bottles, before eating and before contact with young children.
- Leave food, drinks or personal items like car keys, cell phones and mp3 players outside of the laboratory. These items may become contaminated if you bring them into the laboratory or touch them while working in the laboratory.
- Wear a lab coat or other protective garment over personal clothing when working in a microbiology laboratory. Remove protective garment before leaving for non-laboratory areas (e.g., cafeteria, library, or administrative offices). Dispose of protective garment appropriately or deposit it for laundering. Lab coats should be removed from the laboratory only when they are to be laundered by the institution.
- If you work with Salmonella bacteria in a microbiology laboratory, be aware that these bacteria can make you sick. Watch for symptoms of Salmonella infection, such as diarrhea, fever, and abdominal cramps. Call your health care provider if you or a family member has any of these symptoms.
Advice to Laboratory Directors, Managers, and Faculty Involved with Clinical and Teaching Microbiology Laboratories
- A comprehensive set of biosafety guidelines for work with Salmonella and other similar human pathogens can be found in the Biosafety Level 2 section of the CDC/NIH Biosafety in Microbiological and Biomedical Laboratories manual, the Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories MMWR Supplement, and the Guidelines for Biosafety Laboratory Competency MMWR Supplement.
- Either non-pathogenic or attenuated bacterial strains should be used when possible, especially in teaching laboratories. This practice will help reduce the risk of students and/or their family members becoming ill.
- Persons working with infectious agents, including Salmonella bacteria, must be aware of potential hazards and trained and proficient in the practices and techniques required for handling such agents safely.
- Advise all persons working in the laboratory to watch for symptoms of Salmonella infection, such as diarrhea, fever, and abdominal cramps, and to call their health care provider if they or a family member have any of these symptoms.
- All students and employees using the laboratory should be trained in biosafety practices.
- Ensure that handwashing sinks have soap and paper towels. Require students and employees to wash their hands before leaving the laboratory.
- Do not allow lab coats to leave the microbiology laboratory, except to be cleaned by the institution.
- Do not allow food, drinks or personal items like car keys, cell phones and mp3 players to be used while working in the laboratory or placed on laboratory work surfaces.
- Provide students with dedicated writing utensils, paper, and other supplies at each laboratory station. These items should not be allowed to leave the laboratory.
Key Resources
- Guidelines for Biosafety Laboratory Competency, MMWR Supplement
- Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories
- Biosafety in Microbiological and Biomedical Laboratories (BMBL) 5th Edition
- Hand Hygiene in Healthcare Settings
- Handwashing: Hand Hygiene Saves Lives
Final Case Count Map
Persons infected with the outbreak strain of Salmonella Typhimurium, by state, as of June 29, 2011 (n=109)
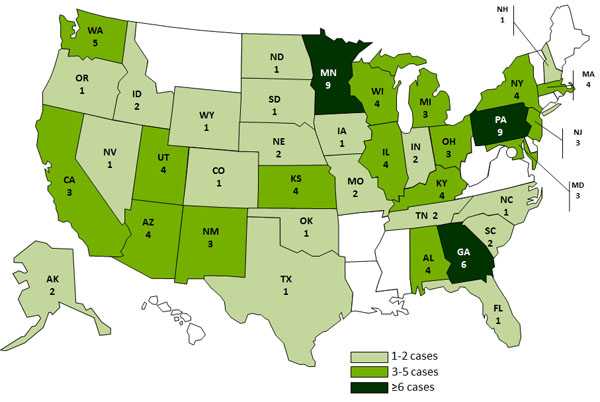
Between August 20, 2010 and June 29, 2011, a total of 109 individuals infected with strain X of Salmonella Typhimurium were reported from 38 states: AK (2), AL (4), AZ (4), CA (3), CO (1), FL (1), GA (6), IA (1), ID (2), IL (4), IN (2), KS (4), KY (4), MA (4), MD (3), MI (3), MN (9), MO (2), NC (1), ND (1), NE (2), NH (1), NJ (3), NM (3), NV (1), NY (4), OH (3), OK (1), OR (1), PA (9), SC (2), SD (1), TN (2), TX (1), UT (4), WA (5), WI (4), and WY (1).
Final Epi Curve
Persons infected with the laboratory strain of Salmonella Typhimurium, by month of illness onset*
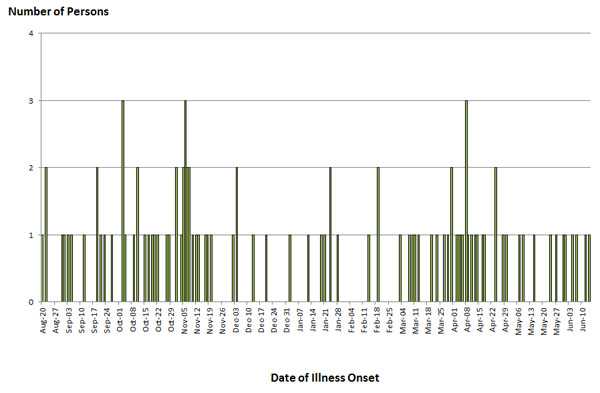
*n=99 for whom information was available as of June 29, 2011. Onset data not currently available for all persons with reported illness.
- Page last reviewed: January 11, 2012
- Page last updated: January 11, 2012
- Content source:


 ShareCompartir
ShareCompartir